Get the job you really want.
Maximum of 25 job preferences reached.
Top Tech Jobs & Startup Jobs
Healthtech • Pharmaceutical
The Financial Assistance Specialist manages billing and collections for copay assistance programs, identifies trends and errors, processes claims, and ensures accuracy in billing and documentation.
Top Skills:
Cpr+Cpt4Hcn 360HcpcsIcd9MS Office
Healthtech • Pharmaceutical
The Authorization Specialist II oversees authorization requests and renewals for specialty pharmacy, manages team performance, and ensures compliance with guidelines while providing mentorship and support to staff.
Top Skills:
MS Office
Healthtech • Pharmaceutical
The Payment Specialist processes payments, refund requests, analyzes contracts, identifies payer trends, and communicates effectively with patients and payers. Requires knowledge of billing procedures and medical terminology.
Top Skills:
CaretendCpr+Hcn 360Patient Accounting Systems
Healthtech • Pharmaceutical
The Onboarding Specialist will promote medication management solutions, conduct phone-based assessments, manage patient relationships, and maintain accurate data entry to grow ExactCare's patient base.
Top Skills:
MS Office
Healthtech • Pharmaceutical
The Onboarding Coordinator manages activities for specialty patients, including patient communication, medication setup, documentation, and ensuring quality customer service under a pharmacist's supervision.
Top Skills:
Microsoft Suite
New
Cut your apply time in half.
Use ourAI Assistantto automatically fill your job applications.
Use For Free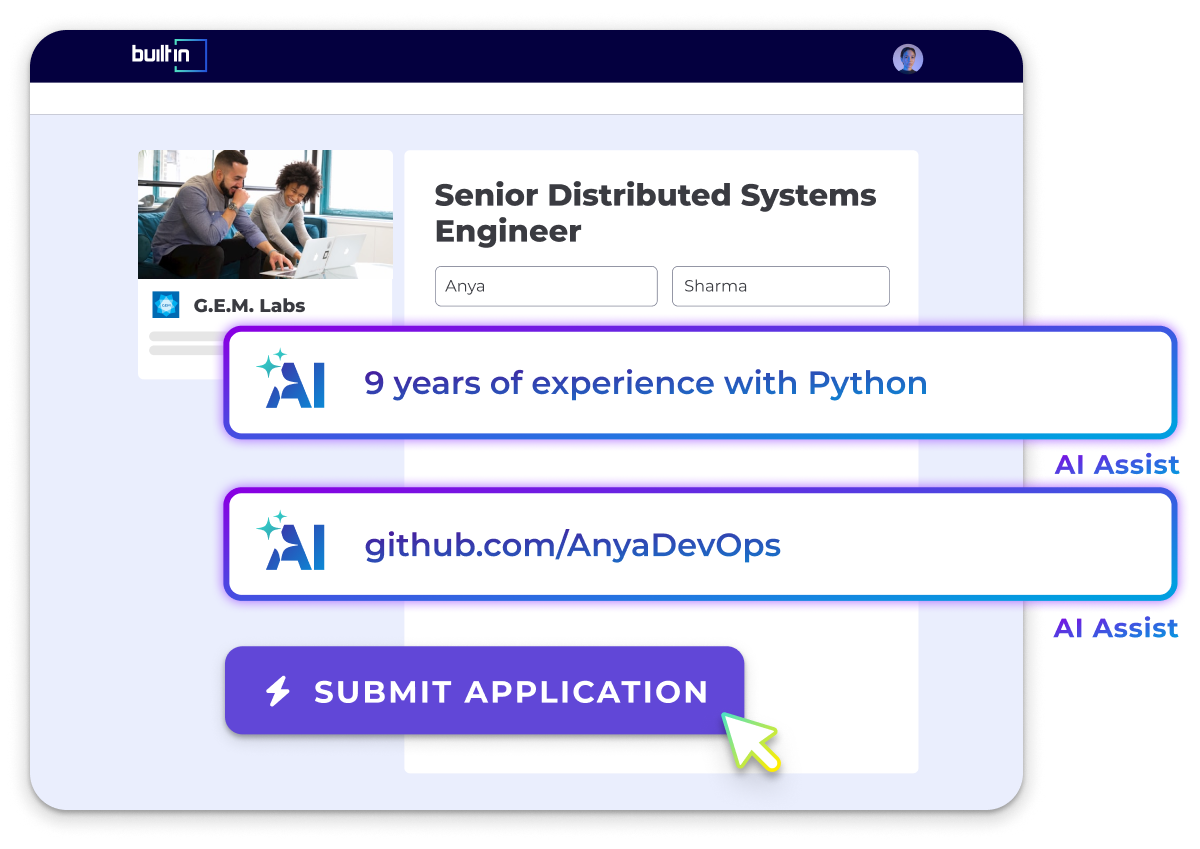
Healthtech • Pharmaceutical
The Onboarding Coordinator supports the specialty pharmacy team by managing patient information, coordinating deliveries, and communicating with patients and healthcare staff under the supervision of a licensed pharmacist.
Top Skills:
Microsoft Suite
Healthtech • Pharmaceutical
The Manager, Payor Relations oversees strategic partnerships, negotiates contracts with payors, ensures compliance, and leads operations within healthcare services.
Healthtech • Pharmaceutical
The Business Unit Specialist manages patient management systems, ensuring revenue cycle accuracy, coordinating projects, and providing analytical support.
Top Skills:
Microsoft 365
Healthtech • Pharmaceutical
Manage daily insurance verification functions, including patient data entry, coverage verification, prior authorizations, and coordination of financial assistance while maintaining productivity and customer satisfaction.
Top Skills:
Microsoft Office Products
Healthtech • Pharmaceutical
The Resupply Specialist handles high volume calls, processes supply orders, verifies insurance benefits, and coordinates with various departments while assisting at the front desk.
Top Skills:
BrightreeSnap
Top Companies Hiring
See AllPopular Job Searches
Tech Jobs & Startup Jobs
Hybrid Jobs
Remote Tech Jobs
.NET Developer Jobs
Account Executive (AE) Jobs
Account Manager (AM) Jobs
Accountant Jobs
Accounting Manager Jobs
Administrative Assistant Jobs
Aerospace Thermal Engineering Jobs
AI Engineer Jobs
Analysis Reporting Jobs
Analytics Jobs
Android Developer Jobs
Application Security Engineer Jobs
Art Director Jobs
Artificial Intelligence Jobs
Assistant Controller Jobs
Associate Product Manager Jobs
Automation Engineer Jobs
Backend Developer Jobs
Blockchain Developer Jobs
Brand Manager Jobs
Business Analyst Jobs
Business Development Manager Jobs
Business Intelligence Jobs
Business Systems Analyst Jobs
C# Jobs
C++ Jobs
Chief of Staff Jobs
Chief Operating Officer Jobs
Cloud Architect Jobs
Cloud Engineer Jobs
Cloud Security Engineer Jobs
Communications Specialist Jobs
Community Manager Jobs
Compliance Analyst Jobs
Content Creator Jobs
Content Jobs
Content Manager Jobs
Content Writer Jobs
Controller Jobs
Copywriter Jobs
Cost Accountant Jobs
Creative Director Jobs
Customer Service Representative Jobs
Customer Success Jobs
Customer Success Manager Jobs
Cyber Security Analyst Jobs
Cyber Security Engineer Jobs
Cyber Security Jobs
Data & Analytics Jobs
Data Analyst Jobs
Data Engineer Jobs
Data Management Jobs
Data Science Jobs
Database Administrator Jobs
Design Engineer Jobs
Desktop Support Jobs
DevOps Engineer Jobs
DevOps Jobs
DevSecOps Engineer Jobs
Director of Engineering Jobs
Director of IT Jobs
Director of Operations Jobs
Editor Jobs
Electrical Engineering Jobs
Embedded Software Engineer Jobs
Engineering Jobs
Engineering Manager Jobs
Environmental Engineering Jobs
Executive Assistant Jobs
Field Engineer Jobs
Field Service Technician Jobs
Finance Jobs
Finance Manager Jobs
Financial Analyst Jobs
Front End Developer Jobs
Full Stack Developer Jobs
Game Designer Jobs
Game Developer Jobs
General Manager Jobs
GIS Analyst Jobs
Golang Jobs
Graphic Designer Jobs
Hardware Engineer Jobs
HR Jobs
Industrial Engineering Jobs
Instructional Designer Jobs
iOS Developer Jobs
IT Jobs
IT Manager Jobs
IT Support Specialist Jobs
IT Systems Administrator Jobs
Java Developer Jobs
Javascript Jobs
Legal Jobs
Linux Jobs
Linux Systems Administrator Jobs
Machine Learning Engineer Jobs
Machine Learning Jobs
Management Trainee Jobs
Manufacturing Engineer Jobs
Marketing Analyst Jobs
Marketing Assistant Jobs
Marketing Associate Jobs
Marketing Coordinator Jobs
Marketing Jobs
Marketing Manager Jobs
Mechanical Engineering Jobs
Network Administrator Jobs
Network Engineer Jobs
Office Administrator Jobs
Office Coordinator Jobs
Office Manager Jobs
Operations Analyst Jobs
Operations Jobs
Operations Manager Jobs
Payroll Specialist Jobs
PHP Developer Jobs
Process Engineer Jobs
Product Analyst Jobs
Product Designer Jobs
Product Manager Jobs
Product Marketing Manager Jobs
Product Owner Jobs
Program Coordinator Jobs
Program Director Jobs
Program Manager Jobs
Project Coordinator Jobs
Project Engineer Jobs
Project Manager Jobs
Prompt Engineering Jobs
Python Jobs
QA Jobs
Quality Manager Jobs
Receptionist Jobs
Research Associate Jobs
Robotics Engineer Jobs
Ruby on Rails Jobs
Sales Development Representative Jobs
Sales Development Representative Jobs
Sales Engineer Jobs
Sales Jobs
Sales Leadership Jobs
Sales Manager Jobs
Sales Operations Jobs
Sales Representative Jobs
Salesforce Administrator Jobs
Salesforce Developer Jobs
Scala Jobs
Scrum Master Jobs
Security Engineer Jobs
Service Desk Analyst Jobs
Sharepoint Developer Jobs
Site Reliability Engineer Jobs
Social Media Coordinator Jobs
Social Media Manager Jobs
Software Engineer Jobs
Software Engineering Manager Jobs
Solutions Architect Jobs
SQL Developer Jobs
Staff Accountant Jobs
Structural Engineer Jobs
Supply Chain Manager Jobs
Support Engineer Jobs
System Engineer Jobs
Systems Administrator Jobs
Systems Analyst Jobs
Tech Support Jobs
Technical Program Manager Jobs
Technical Support Analyst Jobs
Technical Support Engineer Jobs
Technical Support Representative Jobs
Technical Writer Jobs
Test Engineer Jobs
UX Designer Jobs
Web Designer Jobs
Web Developer Jobs
US Jobs
Tech Jobs & Startup Jobs in Albuquerque, NM
Tech Jobs & Startup Jobs in Ann Arbor, MI
Tech Jobs & Startup Jobs in Atlanta, GA
Tech Jobs & Startup Jobs in Baltimore, MD
Tech Jobs & Startup Jobs in Baton Rouge, LA
Tech Jobs & Startup Jobs in Birmingham, AL
Tech Jobs & Startup Jobs in Boise, ID
Tech Jobs & Startup Jobs in Boston, MA
Tech Jobs & Startup Jobs in Buffalo, NY
Tech Jobs & Startup Jobs in Charleston, SC
Tech Jobs & Startup Jobs in Charlotte, NC
Tech Jobs & Startup Jobs in Chicago, IL
Tech Jobs & Startup Jobs in Cincinnati, OH
Tech Jobs & Startup Jobs in Cleveland, OH
Tech Jobs & Startup Jobs in Columbus, OH
Tech Jobs & Startup Jobs in Dallas, TX
Tech Jobs & Startup Jobs in Dayton, OH
Tech Jobs & Startup Jobs in Denver & Boulder, CO
Tech Jobs & Startup Jobs in Des Moines, IA
Tech Jobs & Startup Jobs in Detroit, MI
Tech Jobs & Startup Jobs in Fayetteville, AR
Tech Jobs & Startup Jobs in Greensboro, NC
Tech Jobs & Startup Jobs in Hampton, VA
Tech Jobs & Startup Jobs in Hartford, CT
Tech Jobs & Startup Jobs in Houston, TX
Tech Jobs & Startup Jobs in Huntsville, AL
Tech Jobs & Startup Jobs in Indianapolis, IN
Tech Jobs & Startup Jobs in Jacksonville, FL
Tech Jobs & Startup Jobs in Kansas City, MO
Tech Jobs & Startup Jobs in Las Vegas, NV
Tech Jobs & Startup Jobs in Lexington, KY
Tech Jobs & Startup Jobs in Lincoln, NE
Tech Jobs & Startup Jobs in Little Rock, AR
Tech Jobs & Startup Jobs in Los Angeles, CA
Tech Jobs & Startup Jobs in Louisville, KY
Tech Jobs & Startup Jobs in Madison, WI
Tech Jobs & Startup Jobs in Memphis, TN
Tech Jobs & Startup Jobs in Miami, FL
Tech Jobs & Startup Jobs in Milwaukee, WI
Tech Jobs & Startup Jobs in Minneapolis, MN
Tech Jobs & Startup Jobs in Nashville, TN
Tech Jobs & Startup Jobs in New Orleans, LA
Tech Jobs & Startup Jobs in New York City, NY
Tech Jobs & Startup Jobs in Ogden, UT
Tech Jobs & Startup Jobs in Oklahoma City, OK
Tech Jobs & Startup Jobs in Omaha, NE
Tech Jobs & Startup Jobs in Orlando, FL
Tech Jobs & Startup Jobs in Palm Bay, FL
Tech Jobs & Startup Jobs in Pensacola, FL
Tech Jobs & Startup Jobs in Peoria, IL
Tech Jobs & Startup Jobs in Philadelphia, PA
Tech Jobs & Startup Jobs in Phoenix, AZ
Tech Jobs & Startup Jobs in Pittsburgh, PA
Tech Jobs & Startup Jobs in Portland, OR
Tech Jobs & Startup Jobs in Portland, ME
Tech Jobs & Startup Jobs in Providence, RI
Tech Jobs & Startup Jobs in Provo, UT
Tech Jobs & Startup Jobs in Raleigh, NC
Tech Jobs & Startup Jobs in Reno, NV
Tech Jobs & Startup Jobs in Richmond, VA
Tech Jobs & Startup Jobs in Rochester, NY
Tech Jobs & Startup Jobs in Sacramento, CA
Tech Jobs & Startup Jobs in Salt Lake City, UT
Tech Jobs & Startup Jobs in San Antonio, TX
Tech Jobs & Startup Jobs in San Diego, CA
Tech Jobs & Startup Jobs in San Francisco, CA
Tech Jobs & Startup Jobs in San Luis Obispo, CA
Tech Jobs & Startup Jobs in Santa Cruz, CA
Tech Jobs & Startup Jobs in Seattle, WA
Tech Jobs & Startup Jobs in Spokane, WA
Tech Jobs & Startup Jobs in St. Louis, MO
Tech Jobs & Startup Jobs in Tallahassee, FL
Tech Jobs & Startup Jobs in Tampa Bay, FL
Tech Jobs & Startup Jobs in Tucson, AZ
Tech Jobs & Startup Jobs in Tulsa, OK
Tech Jobs & Startup Jobs in Washington, DC
Tech Jobs & Startup Jobs in Wichita, KS
Tech Jobs & Startup Jobs in Wilmington, NC
International Jobs
Tech Jobs & Startup Jobs in Bangalore
Tech Jobs & Startup Jobs in Brazil
Tech Jobs & Startup Jobs in Czechia
Tech Jobs & Startup Jobs in Germany
Tech Jobs & Startup Jobs in Hungary
Tech Jobs & Startup Jobs in India
Tech Jobs & Startup Jobs in Israel
Tech Jobs & Startup Jobs in Italy
Tech Jobs & Startup Jobs in Japan
Tech Jobs & Startup Jobs in Malaysia
Tech Jobs & Startup Jobs in Mexico
Tech Jobs & Startup Jobs in Netherlands
Tech Jobs & Startup Jobs in New Zealand
Tech Jobs & Startup Jobs in Poland
Tech Jobs & Startup Jobs in Romania
Tech Jobs & Startup Jobs in Spain
Tech Jobs & Startup Jobs in the Philippines
Tech Jobs & Startup Jobs in Turkey
All Filters
Total selected ()
No Results
No Results



